Pathological description
In order to adapt to the increased pressure placed on it, the bone structure deforms and forms growths (osteophytes). The metabolism of the hip joint deteriorates, which negatively affects the muscle and ligament-tendon apparatus of the joint.
degree
| Severity of Hip Arthropathy | Characteristic symptoms and radiographic signs |
|---|---|
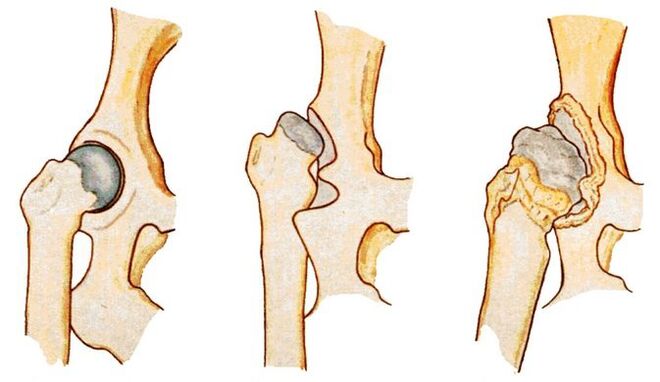
| first | The joint space narrows unevenly and a single osteophyte forms around the acetabulum. Mild discomfort occurs, but more often the disease has no clinical manifestations |
| second | The joint space is almost doubled, the femoral head is displaced, deformed, enlarged, and bone growth is even found outside the cartilage lip. Hip pain persists with significant limitation of movement |
| third | Complete or partial fusion of the joint space, multiple bone growths, and expansion of the femoral head. The pain occurs day and night and spreads to the thighs and calves. Can only move with the help of a cane or crutch |

disease cause
- Previous injury - fracture or dislocation of femoral neck or pelvis;
- hip dysplasia;
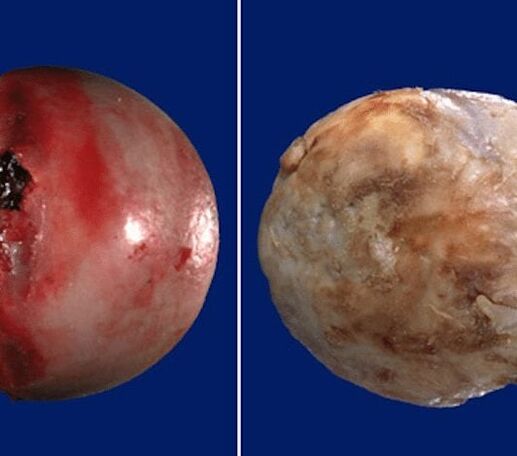
- Aseptic necrosis of femoral head;
- Congenital hip dislocation;
- Inflammation, including infectious diseases of the joints (rheumatoid, reactive arthritis, gout, tendonitis, bursitis, synovitis).
disease symptoms
Limited joint movement
As the disease progresses, morning stiffness and joint swelling become common. In order to regain mobility, a person must warm up for several minutes. By lunchtime, range of motion is restored due to the production of hormone-like substances in the body.
austerity
pain
muscle spasms
limp
shortened legs
diagnosis method
X-ray examination

CT scan
Magnetic resonance imaging

Leg length measurement
laboratory research

hip puncture
Treatment programs
drug
blockade
injection
diet therapy
Sports therapy and massage
physiotherapy




































